Parotidectomy
Pathologies affecting the parathyroid glands are relatively common, affecting women preferentially (3 women for 1 man) after the age of 50. Often discovered by chance, or sought after in the follow-up of identified personal or family pathologies, surgery is in the vast majority of cases the reference treatment for these glands located at the base of the neck. As a professional specializing in surgery of the face and neck, the ENT surgeon is an indicated referent in the care of patients suffering from surgical parathyroid pathology.
Find out more about parathyroid gland surgery from Dr. Delagranda, ENT and cervico-facial surgeon in La Roche-sur-Yon, Vendée.
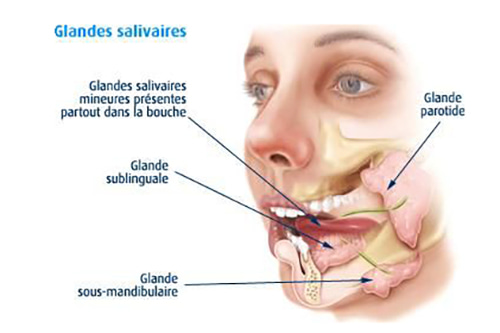
Parotid glands
The 2 parotid glands are exocrine glands (exocrine means product of secretion outside the internal body ie the mouth) which produce saliva mainly during meals, accounting for 30% of saliva in the mouth. They are located in the face on either side of the posterior cheek, in front of and below the ear. They are 5 to 6 cm long, weigh 25-30 g each, and end in a saliva-excreting canal called the Stensen (Stenon in French) duct, which is 4 cm long, 1.5-2 mm in diameter, and terminates in the cheek opposite the 2nd upper molar. The Stenon duct is bifid in 6.9% of cases. The parotid gland is a delicate surgical site, as it is crossed by the facial nerve (nerve of the facial muscles). Parotid glands can increase in volume considerably depending on eating habits (heavy beer drinkers and bread eaters), which does not constitute a pathology. But the parotid glands can also be the site of serious medical problems of tumoral (benign or malignant), infectious (including juvenile recurrent parotitis) or lithiasis (salivary calculi) origin. They may also be the target of more general, systemic pathologies (rheumatoid arthritis, Gougerot Sjögren’s disease, lupus, scleroderma, vascularitis, side effects of radioactive iodine treatment after thyroid cancer). Parotid tumours are benign in 75-80% of cases in adults, but only in 50% of cases in children. There are no risk factors for parotid cancer, apart from patients who have received radiation for another nearby cancer. Parotid cancers account for less than 3% of all head and neck cancers.
MRI is the best examination for studying the body of the parotid gland, but CT is more effective for detecting lithiasis and lymph nodes. Ultrasound is a screening test that can be combined with a cytopunction, which is useful in cases where it is difficult to make a decision (very old people, in poor general condition).
Who is concerned by parotidectomy?
Parotidectomy mainly concern adults of all ages. Children are very rarely concerned.
- Appearance of a persistent mass at the back of the cheek, below or in front of the ear. This mass corresponds to a tumor, most often benign in 75-80% of cases, but sometimes cancerous in 20-25% of cases in adults and 50% in children (source Refcor). Apart from the appearance of a facial mass, there are often few signs: pain is rare and nerve paralysis exceptional (asymmetry of the 2 half-faces). An ultrasound cytopunction of the intra-glandular mass may be suggested to help differentiate between benign and malignant tumors. The most common benign tumor is the pleomorphic adenoma or mixed tumor.
- Presence of a chronic infection of the submandibular gland with chronic disabling pain in the posterior part of the face. Repeated acute infections progressing to chronic infection are most often due to stenosis of the stenon duct or a trapped calculus. If the stone cannot be treated by lithotripsy, sialendoscopy, combined approach (please link to the nathan sialendoscopy page) or endo-buccal excision, the only solution is to remove at least part of the gland: a parotidectomy. Stenosis of the stensen duct may be dilated or operated on, but parotidectomy remains a possibility.
- Swelling of the salivary gland at mealtimes, with pain (salivary colic) or without pain (salivary hernia). These symptoms can be linked to a calculus/lithiasis or stenosis of Stenon’s canal, or a salivary calculus in the parotid gland itself. If the calculus cannot be treated by lithotripsy, sialendoscopy (link to the nathan sialendoscopy page please), the combined approach or endo-buccal excision, the only solution is to remove at least part of the gland: a parotidectomy.
Objectives of parotidectomy
- Stop pain (stones, stenosis).
- Stop recurrent infections (parotitis).
- Prevent the spread of cancer by removing it.
- Prevent the troublesome development of a benign tumor
The different stages of the intervention
The surgical procedure
The gland can be partially or totally removed, depending on the indications.
Parotidectomy is always performed under general anaesthetic with tracheal intubation. It can be performed in 90 minutes or more. The cervico-facial incision is 8-9 cm long, in front of the tragus of the ear, then under and behind the ear. It then descends into a fold in the neck, 2 cm from the angle of the mandible. Parotid surgery is performed by monitoring the facial nerve’s response to stimulation, by monitoring facial muscle activity.
Parotidectomy is combined with cervical lymph node curage in the case of cancer only. A drain is placed in the parotid area at the end of the operation to limit the risk of post-operative hematoma.
Post-surgery recovery period
The patient returns home after an average of 2 or 3 days in hospital. Pain is minimal. Eating can be a little tricky at first, but improves very quickly, due to the proximity of the jaw joint.
10 days off work.
Post-operative care at home: Daily nursing care of scar.
Scar: 8-9 cm on the face and neck, barely visible from the front. Protect from the sun.
Complications associated with parotid gland surgery
In addition to the risks inherent in any surgery involving general anaesthesia, parotidectomy carries the risk of more or less rare complications:
- Post-operative hematoma.
- Anesthesia of the earlobe or auricle due to damage to the auriculotemporal nerve.
- Facial asymmetry in mimicry due to damage to the facial nerve, which is highly sensitive to stretching. This facial paralysis of variable intensity regresses over time, except in the case of nerve sectioning. The eye must be well protected, as the eyelids do not close.
- Redness and sweating of the cheek when eating certain foods. Called Lucy Frey syndrome, it corresponds to aberrant reinnervation during healing. It can be improved with scopolamine patches or botulinum toxin injections. There is no preventive treatment or special precautions to avoid it.
You may notice a slight depression behind the jaw angle after the operation. This is not a complication, but a consequence of the absence of the removed gland.
For further explanations, please consult the College of ENT’s explanatory sheet on parotidectomy :
Frequently asked questions
Here is a selection of questions frequently asked by Dr Delagranda’s patients during consultations for parotidectomy in La Roche-sur-Yon.
Will it be difficult for me to eat?
Sometimes for a few days.
Will I still have saliva?
Yes, because there are 5 other main salivary glands and a thousand accessory salivary glands.
Will I be able to move my face again?
Yes, if the nerve has not been cut, but it may take a long time (weeks). The labial commissure area is often the last to recover. Persistent facial paresis is exceptional when the nerve has not been cut.
Fees and cost of the operation
Parotidectomy surgery is covered by the French health insurance system. Contact your mutual insurance company to find out whether any extra fees will be covered.
Do you have a question? Need more information?
Dr Antoine Delagranda will be happy to answer any questions you may have about parotidectomy. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.
ENT consultation for a parotidectomy in Vendée
Dr Antoine Delagranda will be happy to answer any questions you may have about parotidectomy. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.

