Sialendoscopy
Sialendoscopy is a recent, minimally invasive interventional technique that enables the diagnosis and treatment of salivary gland pathologies in the same operating time by endoscopy of the salivary ducts. It is particularly effective on obstructive disorders of the salivary excretory ducts of the parotid and sub-maxillary glands, such as stenosis and calculi (lithiasis). It can be used in adults of all ages, and in children over 3. It reduces the number of indications for salivary gland removal by up to 5%.
Find out more about sialendoscopy from Dr. Delagranda, ENT surgeon in La Roche sur Yon, France.
Who is concerned by sialendoscopy?
Adults of all ages (97% of cases) may be concerned by salivary lithiasis or calculi and salivary stenosis, and children from the age of 3 (3% of cases). The average age of discovery of lithiasis is 41 for the sub-maxillary gland and 48 for the parotid gland.
Certain pathologies or sequelae of rare treatments may also warrant sialendoscopy.
Children may suffer repeated parotitis as part of juvenile recurrent parotitis, a pathology little-known to doctors, which peaks between the ages of 3 and 7. It is the second most common salivary disease in children, after Mumps.
Patients who have undergone radioactive iodine treatment for thyroid cancer sometimes experience disabling salivary symptoms.
Patients who have had radiotherapy to the cheeks
Patients with Gougerot Sjögren’s disease, scleroderma, lupus, rheumatoid arthritis and certain thyroid conditions may also experience troublesome salivary symptoms.
Patients who have had a face-lift.
A foreign body accidentally trapped in a salivary duct
Sialendoscopy can help in these rare cases
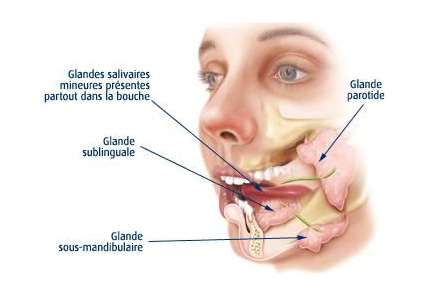
Salivary glands
There are 6 main salivary glands: 2 parotid glands in the cheeks, 2 submandibular glands under the lower jaw, and 2 sublingual glands under the tongue in the floor of the mouth. There are also around 1,000 microscopic accessory glands distributed throughout the mouth and pharynx. Only the parotid and submaxillary glands are accessible for sialendoscopy, as their excretory ducts are of sufficient diameter. The excretory canal of the parotid gland is called Stensen’s canal (Sténon in French), 1.5-2mm in diameter and 4cm long, and emerges from the inner surface of the cheek in an orifice called the papilla, opposite the 2nd molar. The excretory duct of the sub-maxillary gland is called Wharton’s duct, 2-3mm in diameter and 4-5cm long, and exits under the tongue behind the incisors into an orifice called the papilla at the level of the wattles. The ducts of the other glands are too small to be explored. Saliva is mainly produced continuously by the submandibular glands (70%), and especially during meals by the parotid glands (30%). The salivary glands can be the site of acute or chronic infection (sialadenitis), painful swelling (salivary colic) or swelling without pain (salivary hernia), most often at mealtimes. Obstruction of saliva flow is generally due to calculi in 66% of cases, stenosis in 33% and extrinsic compression in 1% , but percentages are different according to the gland.
L.S.D. Classification (Lithiasis, Stenosis, Dilatation)
In 2008, members of the European Salivary Gland Society proposed the first classification of pathologies visible in sialendoscopy. This classification takes into account the specificities of sialendoscopy techniques and medical practice.
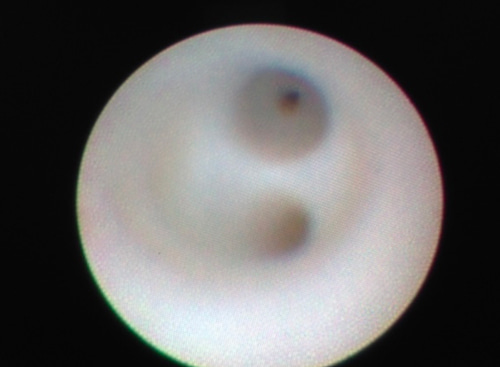
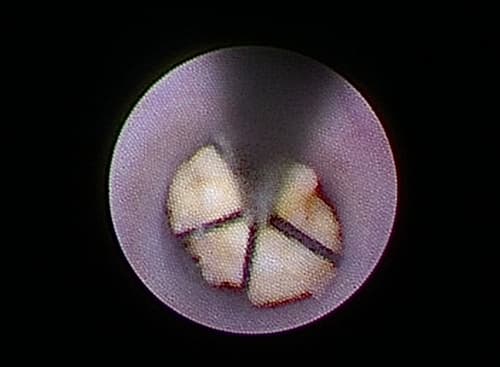
- For calculi, the criterion of presence or absence of mobility within the duct is paramount, as a mobile calculus is much more likely to be removed by sialendoscopy. In the case of immobile or embedded calculi, successful removal depends on whether they can be fragmented (by laser or impulse shock), so the most important criterion is their visibility within the canal. Whether or not the stone is palpable is an indication of whether a combined approach is more feasible (sialendoscopy to help locate the stone and check cleanliness after extraction + endooral opening and dissection to look for the stone to extract).
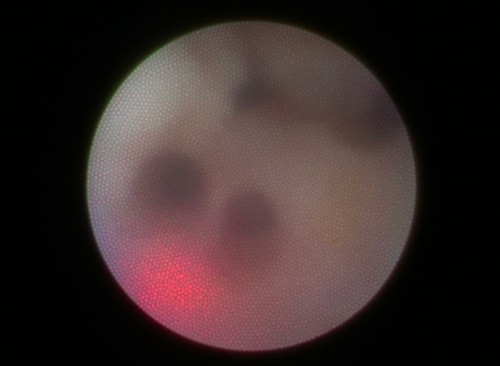
- Stenoses may concern a secondary or main salivary duct, and may be localized, extensive or even diffuse: the classification describes the different possibilities of stenosis. The difficulty of resolving stenoses is generally correlated with the classification (S1 = easier, S4= very difficult).
- Salivary duct dilatations, or ectasia, may be single or multiple, and lie upstream of the stenosis.
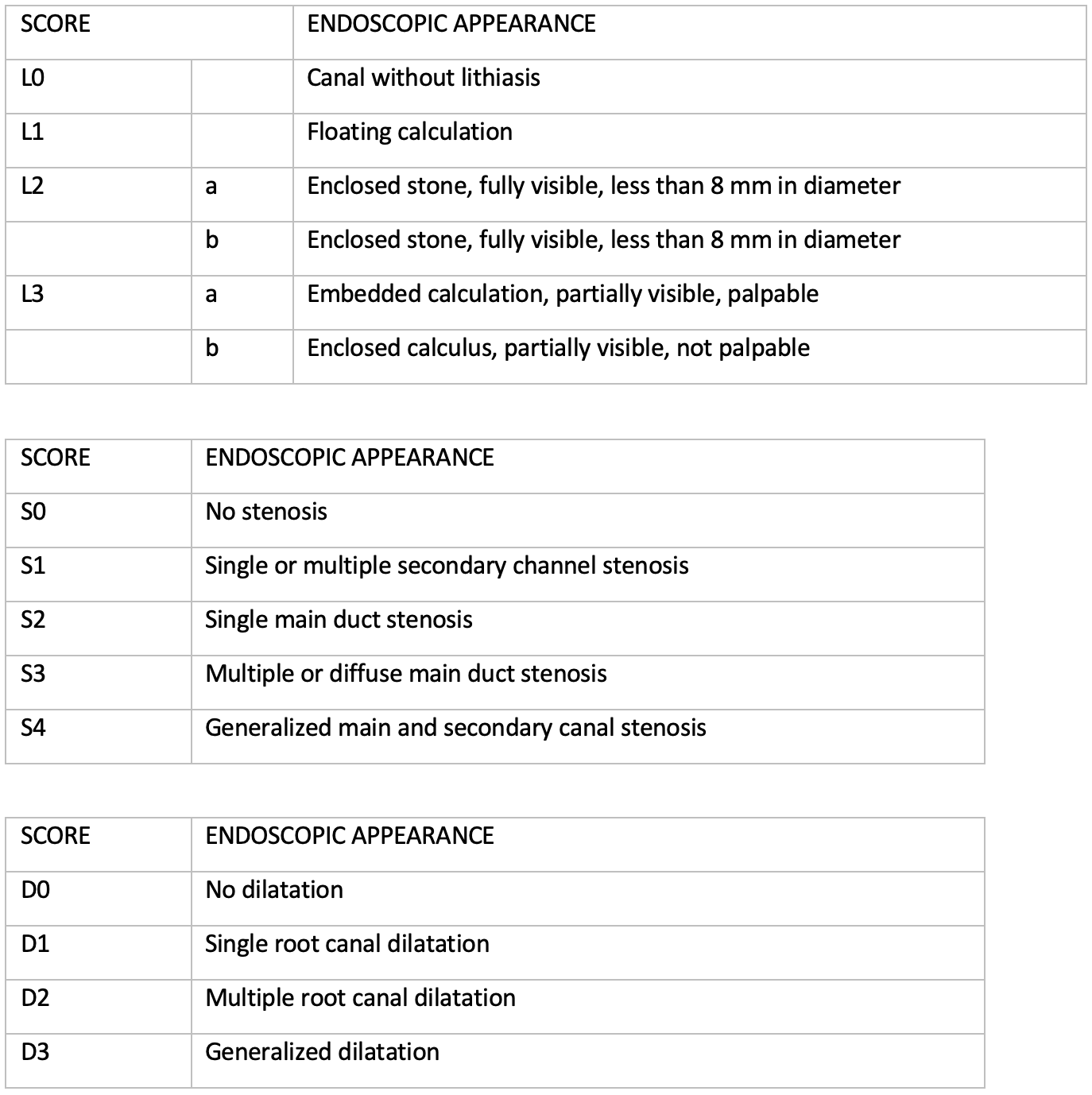
A sialendoscopy operative report may therefore include an LSD classification result (e.g. L1S0D0).
When should a sialendoscopy be performed?
Indications for sialendoscopy are highly specific and depend on a number of criteria: the gland(s) concerned, the number, location and size of stones or strictures, previous history, medication taken, clinical context (infection or not), jaw shape, position and size of teeth, depth of oral floor, presence of ranula or mandibular torus. Your surgeon will be able to guide you in this decision.
What signs might prompt me to consult a surgeon for a sialendoscopy?
- Rapid painless swelling at mealtimes in front of the ear or under the jaw, which diminishes fairly rapidly (salivary hernias)
- Painful swelling at mealtimes in front of the ear or under the jaw, which diminishes very slowly (salivary colic).
- A permanent feeling of heaviness under the jaw
- Repeated infections of the salivary glands (parotitis or maxillitis)
- The chance discovery of lithiasis/calculi during an examination carried out for another reason (dental panoramic, facial scanner, cervical ultrasound, cervical MRI).
It’s important to know that stones affect 1/7500 people, and can remain asymptomatic for a long time. Many are eliminated spontaneously with the saliva (small, very hard, yellow or white elements a few mm in size, found in the saliva). Their average size is 3.2 mm in the parotid gland and 4.9 mm in the sub-maxillary gland. However, some are symptomatic as small as 2 mm in diameter, and can remain trapped, increasing inexorably in size by 1 mm per year until they cause painful and increasingly frequent symptoms. It is preferable to remove these persistent stones when they are small, even if they have not yet become symptomatic. In up to 30% of cases, multiple stones can be found in the same or another gland. Lithiasis is radiopaque (visible on X-ray or CT scan) in 90% of cases.
Objectives of sialendoscopy
- Reduce the number of salivary gland infections (sialadenitis, parotitis, submaxillitis)
- Reduce salivary gland swelling (salivary hernias)
- Reduce salivary gland pain (salivary colic)
- Extraction of salivary calculi/lithiasis, mucous plugs, occlusive polyps, foreign bodies
- Dilation of salivary strictures

The different stages of the intervention
Surgical intervention
It’s important to be well hydrated the day before surgery (1.5-2 liters of water) to facilitate the surgical procedure, by increasing the flow and volume of saliva excreted.
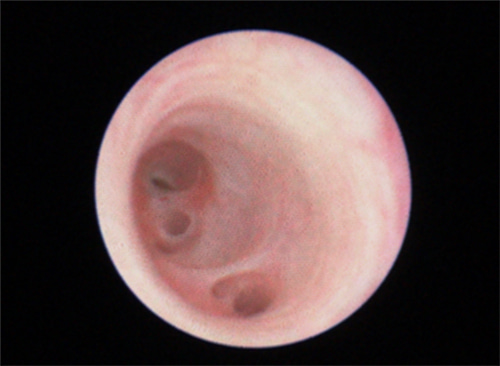
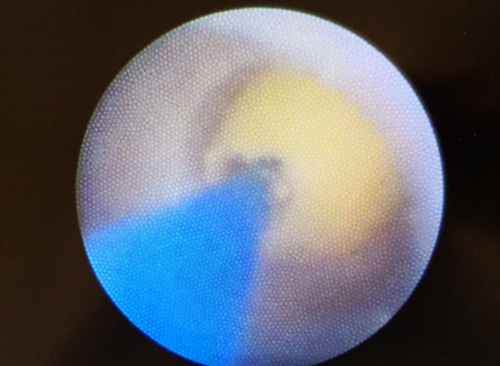
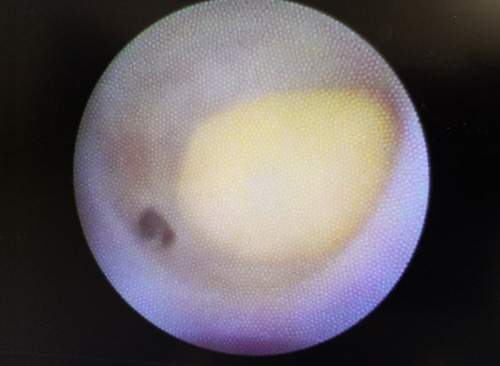
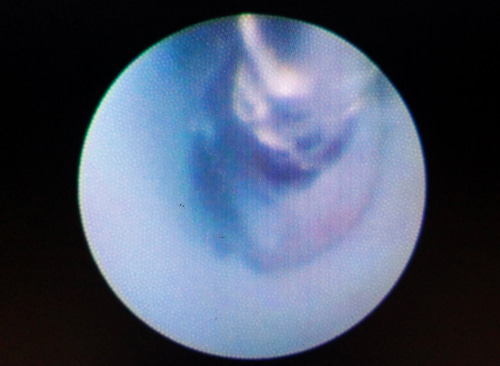
During sialendoscopy, a small endoscope is placed in the diseased salivary gland(s) via the saliva excretory ducts in the mouth. The sialendoscope, which ranges in size from 0.7 to 1.6 mm, can be used to dilate stenoses (balloons), dislocate stones (laser or pulse) and remove them (basket probe). Sialendoscopy can also be combined with a more conventional approach in difficult cases, to increase safety or check the validity of the procedure performed: this technique is called a combined approach. Sialendoscopy is performed under general anesthesia, more rarely under local anesthesia, and most often on an outpatient basis.
Sialendoscopy can be performed on several salivary glands at the same time, without limitation.
It is not uncommon for a silicone healing stent to be left in place in the operated salivary duct for 10 to 21 days. It is easily removed at a later stage in the office.
In special cases, extracorporeal lithotripsy prior to sialendoscopy may be proposed.
Post-surgery recovery period
The patient returns home on the same day as an outpatient. Pain is minimal. The cheek or area under the jaw may be very swollen on the day of the operation, but will return to its original appearance within 48-72 hours.
Post-operative care at home: Moisturize thoroughly to facilitate saliva production. Lemon/orange/grapefruit/tomato juice to stimulate saliva excretion. Daily, gentle self-massage of the gland from back to front is recommended to drain the salivary gland. Mouthwashes are prescribed for 21 days, along with mild analgesics (class I), non-steroidal anti-inflammatory drugs and sometimes antibiotics for 7 days.
Scarring: no visible scar on the face
Complications associated with sialendsocopy
In addition to the risks inherent in any surgery performed under general anaesthetic, sialendoscopy carries the risk of rare complications (3.23%) and failures:
- Stenosis of the salivary duct
- Perforation of the salivary duct
- Ranula: pseudocystic fluid extravasation
- Salivary fistula
- Lingual nerve paralysis
It’s important to know that, despite an experienced surgeon, in 1 to 4% of cases it’s not even possible to enter the salivary duct, making exploration impossible.
For further information, please consult the College of ENT’s explanatory sheet on sialendoscopy:
Frequently asked questions about sialendoscopy
Here is a selection of questions frequently asked by Dr Delagranda’s patients during consultations for sialendoscopy in La Roche-sur-Yon.
Should I prepare myself the day before the operation?
Yes, in addition to the usual preparations (shower, etc.). It is important to drink 1.5-2 litres of water the evening before the operation to encourage saliva production and make the procedure easier.
Are sialendoscopy operations painful?
No, as a general rule you don’t even need to take paracetamol from day one.
Should I stay in hospital for a sialendoscopy?
Unless the surgeon or anaesthetist exceptionally advises otherwise, it is not necessary to sleep in the clinic.
Are there any risks involved in sialendoscopy?
Yes, although it is a purely endoscopic treatment (except in the case of the combined route), there are complications as with any surgery, but they are fewer than with conventional surgery.
Is the operation always successful?
As with any surgical operation, there are risks of failure, depending above all on the indication for the procedure. Sialendoscopy is a highly technical procedure that requires specialised training, a long learning phase and assiduous practice. Your surgeon has validated these steps in order to provide you with the best possible success with the least possible risk.
Do I need to take any medication after the operation?
Yes, depending on the case, your surgeon will have prescribed a painkiller, an anti-inflammatory and an antibiotic.
Are there any precautions to take after the operation?
Yes, you should rinse your mouth, drink plenty of water, eat cold or lukewarm food and avoid chewing on the operated side, especially if the surgeon has placed a temporary stent in the salivary duct.
Fees and coverage of the procedure
Health insurance covers sialendoscopy alone or combined. Contact your health insurance company to find out how much coverage there is for any extra fees.
Do you have a question? Need more information?
Dr Antoine Delagranda will be happy to answer any questions you may have about sialendoscopy.Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.
ENT consultation for sialendoscopy in Vendée
Dr Antoine Delagranda will be happy to answer any questions you may have about sialendoscopy. Dr Delagranda is a specialist in ENT surgery at the Clinique Saint Charles in La Roche-sur-Yon in the Vendée.